|
Background to the History of General Practice in Australia
Australia's First Medicine Men
Australia's First Medicine Men of course were
the Aboriginal medicine men. At the time that James Cook arrive in
Austalia (1760) it is likely that the Australian traditional healers
were better at treating their patients than the English doctors were at
treating theirs. Both could set broken bones and treat wounds tolerably
well. To the English, diseases were due to miasmas (mysterious odours
comig from decaying material), diseased parents, sedentary habits,
emotional upset or environmental conditions such as getting cold or wet.
They had nothing effective in treating them. The Aboriginal medicine
man saw disease as a disturbance of the patient's spirit and sought to
rectify that disturbance. The Aboriginal doctor had a large
pharmacopoeia of active drugs at his disposal. The English doctor had
but a handful of drugs that actually worked, and only one of those
(quinine) was of any use in infectious diseases (malaria) unless one
considers the widespread use of mercurial salts for syphilis as being
useful.
More on the Australian traditional healer can be read here.
The Practice of Medicine in Early England
"The present classification of medical men
is a child of circumstances. In former ages, nay, even within the last
three centuries, there really was but one species of practitioner in
this country. This was the physician; for, although persons practicing
surgery existed before that period, they were a degraded race of men as
far as medicine is concerned. They were only persons exercising the
calling of barbers, who took upon themselves to bleed and draw teeth; to
perform other slight operations in surgery, and ultimately to engage in
the medical care of surgical diseases. hence gradually arose a
corporation of barber-chirurgeons, and after a time of division of this
corporation and the institution of a new one, under the name of
Corporation of Chirurgeons.
With respect to physicians, it is probable
also that they were at first apothecaries or shopkeepers; that is to
say, they dispensed their own medicines. After a time, however, it
became convenient that a separate class of apothecaries should be
formed. But the physician tried to take special care that the apothecary
should be confined to his own calling, and on no account engage in the
practice of medicine. The apothecary, then, held the same situation that
appertains, or ought to appertain, to the present druggist.
Nevertheless, public convenience, which sets at defiance the private
interests of individuals or sets of individuals, called on the
apothecary to prescribe, as well as to dispense medicine. The physicians
took fire at this, and a most virulent and entertaining war took place
about two hundred years ago, between the physician and the apothecary;
the former being actuated by the vain hope of preventing the latter from
obeying the commands of a far superior power. Of course the physician
failed in his object; the apothecary became established as a regular
practitioner; the wants of society, if not the law, sanctioned his
existence, and hence arose the general practioner.
The world never stands still; and as society
in this country did not retrograde, its wants and its improvements went
hand in hand, untill at last the general practitioner became so
extensively engaged in the practice of medicine, that a further division
was found to be convenient, and about thirty years ago, the new order
of druggists arose."
Taken from the Transactions of the Associated Apothecaries and Surgeon- Apothecaries, 18238. |
It should be understood that in England and
particularly London, occupations were controlled by livery companies
(guilds and trade associations) that had features of professions, trade
unions and secret societies. These companies controlled the
trades/professions partly by regulating membership. The practice of
medicine in the era before England colonised Australia was controlled by
three groups:
- The surgeons
- The physicians
- The apothecaries
 |
The surgeons
had their origins with the Guild of Surgeons Within the City of London
in the 14th century. Prior to this, monks were the traditional healers,
however a papal decree forbad them to shed blood. The barbers assisted
the monks and were to perform blood-letting, leeching, drainage of
abscesses, extraction of teeth, enemas, fire cupping, leeching, neck
manipulation, as well as hair cutting and shaving.
In 1462 the Worshipful Company of Barbers was incorporated. There was
a conflict between the surgeons and the barber surgeons until an
agreement in 1493 was signed giving the surgeons the power of
incorporation. They became the Guild of Surgeons. Henry VIII ratified a
combining of the two to become the Company of Barber Surgeons in 1540.
In 1745 the surgeons requested a separation and this was granted by an
act of parliament. They formed the Company of Surgeons. They built a new
hall with an anatomy theatre near Newgate Gaol so it could dissect the
bodies of executed criminals for learning and teaching purposes. In 1800
they became the Royal College of Surgeons (RCS). Although this was
changed to the Royal College of Surgeons of England in 1843, it remained
commonly known by its former name.
|
Because they did not have a formal university education, the surgeons
were not givern the title "Dr", a custom which persists today. 1843
also saw the formation of the higher qualification, the Fellowship of
thge Royal College of Surgeons (FRCS). From the 1800s the examinations
were held in conjunction with the Royal College of Physicians and those
who passed were given the post-nominal, MRCS LRCP (Member of the Royal College of Surgeons, licentiate of the Royal College of Physicians).
| The physicians.
The College of Physicians of London (also known as the King's College)
was founded by royal charter (King Henry VIII) in 1518, following a
petition led by Thomas Linacre. The purpose of the petition was to seek
recognition of trained physicians to distinguish them for the untrained
practitioners that practiced under the same nomenclature. The College's
powers were extended from London to the rest of England in 1523 by an
act of parliament. It became known as the Royal College of Physicians
(RCP)in the 17th century following the re-establishment of the monarchy.
Initially the training was academic and required a demonstrated
classical education as well as an education in medicine. Examinations were viva
voce. There were fewer than sixty fellows (and 100 licentiates) at any
time up until the 19th century. One issue of contention was the
admission to the College of non-Oxbridge trained practitioners. |
 |
It was not until 1835 that practitinoers from other universities
were allowed fellowship. Similarly membership excluded women until 1909.
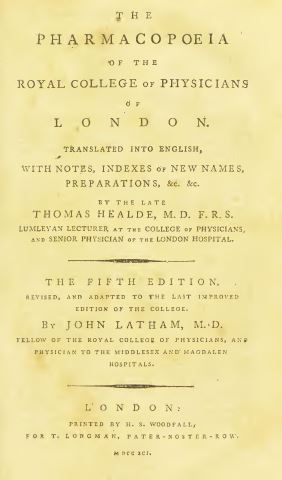
The College published the London Pharmacopoeia in 1618 and this was the first standardised list of medications in England. In 1869 it also published the Nomenclature of Diseases, which became an international standard for naming diseases until the 20th century.
The College previously issued a Licentiate of the Royal College of
Physicians (LRCP), available to Oxbridge medical graduates. This
post-nominal was ceased in 1999. Those passing the RCP examinations were
became Fellows (FRCP).

|
The apothecaries
were descended from the grocers (so named because they bought in
gross quantities). The Grocer's Company was described in 1365 as the "Mistery of
Grossers, Pepperers and Apothecaries". One can imagine that the
apothecaries were those who specialised in the trade of items of
medicinal use. Over time they became the experts in the use of the
substances they traded. Consequently they sought to become a guild of their
own. In 1617 they were granted a royal charter by James I and formed the Worshipful Society of Apothecaries. They challenged the College of Physicians regarding their monopoly in practicing medicine.
|
In 1673 the Society created the Chelsea Physic Garden
(which still exists). This was a place where medicinal plants were
grown and studied. The garden was used to teach medical students botany.
It became one of the most important centres for botany and plant
exchange in the world.
In 1704 the "Rose Case" was a landmark trial. The House of Lords
overturned a prior ruling of the Bench of the Queen and allowed Thomas
Rose (an apothecary) to prescribe. This was seen as a license for all apothecaries to
prescribe. However, they were not allowed to charge for their diagnostic
services, but were only allowed to charge for the medications they
provided. The apothecaries were, therefore allowed to practice medicine.
In 1815 the Apothecaries Act was to give the Society power to license
and regulate medical practitioners throughout England and Wales. It
continued to do this until 1999 (when the Uniting Examination Board was
disbanded). The Society of Apothecaries went on to liaise with the
College of Physicians and eventually together with the College of
Surgeons form conjoint examining bodies for the purpose of registering
medical practitioners. A qualification through the Society of
Apothecaries was the LSA (Licentiate of Apothecaries).
In recent times (1928 - 2002) the Society of Apothecaries offered diplomas in areas not covered by the colleges:
- the Mastery of Midwifery (MMSA)
- Diploma in the Forensic and Clinical Aspects of Sexual Assault
- Diploma in Medical jurisprudence
- Diploma in the History of medicine
- Diploma in GenitoUrinary medicine
- Diploma in the Philosophy of medicine
- Diploma in the Medical care of catastrophes
- Diploma in the Forensic medical sciences
- Diploma in HIV medicine
In the early 1800s the practice of medicine was plagued by charlatans:
unskilled people claiming to be doctors. Those who were trained took
umbrage at this situation and sought to remedy it. The College of
Physicians, the College of Surgeons and the Society of Apothecaries met
to agree on a petition to the government. This resulted in the 1815
Apothecaries Act. The Act set down the requirements for registration as a
doctor. This included an apprenticeship and training in anatomy,
botany, chemistry, materia medica and "physic" (medicine). This act was
the beginning of regulation of the medical profession in England. Up to
this point a doctor could be someone with formal medical education
through the university of Oxford or Cambridge or it could mean someone
who had been apprenticed to an apothecary.
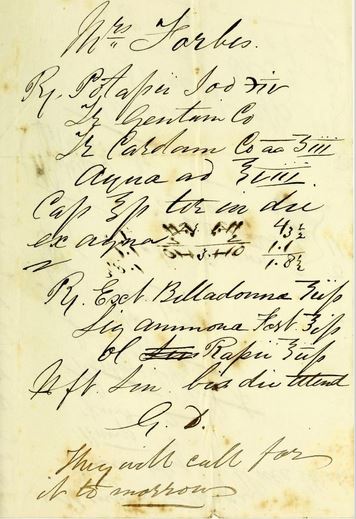
| To gain insight as to the practice of medicine, examine the Materia Medica from the Pharmacopoeia of the Royal College of Physicians of London, published 1791. This contains 239 (mostly herbal) ingredients, which could be used in prescriptions. Whilst today's prescriptions are mostly pre-formulated commercial products, in the 17th and 18th centuries, prescriptions were made up by the apothecary or dispensing chemist from basic ingredients. This link shows how to read these old prescriptions.
|
 |
|
| |