|
The Spanish Flu in Australia
The Spanish Flu was one of the worst pandemics in human history. It is thought to have infected about 500 million people worldwide, ie about one third of the word population. Estimates are that it killed at least 50 million people. Accurate figures were not known because many countries at the time did not keep good medical statistics and the extent in African and many Asian countries was unknown. Recent PCR studies of samples recovered from people who died at the time have shown that it was an influenza A H1N1 strain. The geographic origin of this strain remains unknown and is still widely debated. It almost certainly did not originate in Spain, despite the name. The name arose because of Spain was one of the few "western" countries not under media censorship during World War 1. Little information about the spread of the virus was released in other countries so as not to alarm the populations further and not affect troop morale. Being neutral in the war, Spain had no such censorship and so reported what was happening in its country. As a result, the world had a false impression that the flu was worse in Spain than elsewhere.
The Virus:
Between1999 and 2005, Taubenberger and Reid had coded the whole genome of the Spanish flu RNA1 4. This was possible because the military had on record some pathology specimens (formalin fixed samples embedded on slides) from soldiers who had had the Spanish flu. Another sample came from the exhumed, frozen body of an Inuit woman who died of Spanish flu and had been buried in the permafrost in Alaska. The virus was identified as influenza A, type H1N1.
Influenza A viruses contain only 8 genes which encode for 11 proteins. Because of the small size of the genome and the relative simplicity, there is no coding for mechanisms to repair or error check the RNA. This leaves it susceptible to relatively rapid mutation. The influenza RNA is a negative RNA: it requires conversion to a positive RNA before it can code for proteins.
Influenza A viruses contain 8 physically separate RNA segments that code as follows:
- Segments 1 to 3 code for three different polymerase subunits, which need to combine to combine to form a functional polymerase (to copy RNA within the infected cell)
- Segment 4 encodes for HA (hemagglutinin)
- Segment 5 encodes NP, which is a nucleoprotein
- Segment 6 encodes NA (neuraminidase)
- Segment 7 encodes two matrix proteins (M1 and M2)
- Segment 8 encodes two non-structural proteins (NS1 and NEP)
|
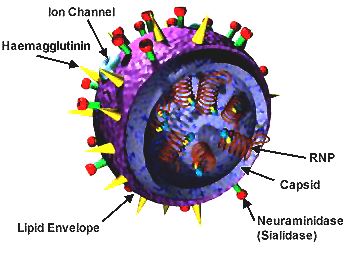
Courtesy: California Dept. of Health Services |
The virus assembles using about 500 molecules of HA, 100 of NA and 3,000 of matrix proteins. HA and NA make up most of the viral coat and hence are the proteins first presented to the host and the proteins responsible for immune response. There are 18 subtypes of HA and 11 subtypes of NA known, but in humans H1, H2, H3, N1 and N2 are most commonly found. The HA protein binds to receptor sites in the host, typically sialic acid. The NA typically cleaves this bound terminal sialic acid group.
Analysis of the genome of the Spanish flu virus was done in order to assess how it evolved. It showed that the virus had some features suggestive of avian flu and some of mammalian flu. The Spanish flu is now considered to be the ancestor of the current H1N1 strains. Unfortunately, genetic anyalysis has neither determined why this influenza was so virulent nor determined its geographic origins.
The State of Medical Knowledge in 1918:
At the time that the Spanish flu was first recognized, it was understood that influenza was an endemic, infectious disease which sometimes flared into epidemics and pandemics: the previous pandemic having been the Russian Flu in 1889 to 1890.
It was recognized that the infective agent was in the sputum and that the young and old were most susceptible to deleterious effects of influenza and should be isolated in order to protect them. Prevailing thought was that influenza was caused by a Gram negative bacillus, isolated by the German pathologist Richard Pfeifer in great numbers from the sputum of patients with influenza in 1892. This was called Bacillus influenzae but is now known as Haemophilus influenzae. Verification of this organism in patients with influenza was made by other doctors. However, other bacteria were sometimes cultured from patients with influenza. Pneumococcus, Streptococcus and Micrococcus (Mycoplasma) were sometimes the dominant bacterium. In some patients with influenza Pfeifer's bacillus (as it came to be known) was not found. Two possibilities were considered:
- that the individual became partially immune to the bacillus after an initial illness and this hindered the ability to culture it on subsequent occasions.
- that the clinical presentation of influenza was not one disease but several diseases with similar presentations.
Debate also continued as to whether B. influenzae was in fact the cause of influenza as it did not meet all of Koch's postulates (Robert Hermann Koch, 1843-1910). These were as follows:
- The microorganism must be found in abundance in all organisms suffering from the disease
- The microorganism must be isolated from a diseased organism and grown in pure culture.
- The cultured microorganism should cause disease when introduced into a healthy organism
- The microorganism must be re-isolated from the inoculated, diseased experimental host and identified as being identical to the original specific causative agent.
The problem was that the organism, when introduced into a new host, did not cause influenza. As well, the bacillus could be found in the throats of individuals who did not have influenza and could be found in other medical conditions such as endocarditis, meningitis and otitis externa. The organism was also found in some patients with chronic bronchitis. Some doctors were calling this condition chronic influenza56.
A second problem, was that the infective organism was not filtered out by filters that removed known bacteria. The filtrate retained the factor which triggered influenza.
Influenza was seen as a disease with a very sudden onset, presenting with headache and pain in the eyeballs, bachace, pain in the limbs, a rapid rise in temperature, prostration and with tachycardia.
Stengel (1911)57 described five types of influenza, depending upn presentation:
- catarrhal. In this type an irritative cough, coryza and conjunctivitis predominate. It may lead to a productive cough with purulent sputum.
- nervous. In this type the headache and various neuralgias dominate with the skin being sensitive to touch. Pain in the extremeties might be present. There would be profound weakness and "mental depression and aberrations". The depression might persist for months.
- gastro-intestinal. In this type there would be unusual prostration, nausea, vomiting and diarrhoea.
- circulatory or cardiac type. This would typically follow on from one of the other four and would manifest as tachycardia, bradycardia, other arrhythmia or heart block. Enocarditis or pericarditis would be rare complications
- typhoid. In this type the fever would be dominant. The spleen could be enlarged. It would be distinguished from typhoid by the lack of severe leucopoenia and the abscence of rose spots.
The Origin of the Spanish Flu:
Because of the war there was more movement of people around the world than had probably ever occurred before in the history of mankind. The lack of good medical records in some countries at the time has prevented good restrospective tracking of the origin of the virus, but even in countries that normally kept good records, statistics were not always accurate:
| "Owing to the extreme pressures of work, the overtaxed state of the medical staff, the variability of nomenclatures in official rerturns, and other similar causes, it has been impossible to keep detailed records of all of the cases encountered" (Dr A. Abrahams, 1919)2. |
One of the biggest difficulties in tracking the origins of the Spanish flu, is the fact that influenza occurred commonly each winter in all countries and there were always deaths associated with it. Determining which deaths were due to the new stain and which were due to previously existing strains has been near impossible. Theories as to the geographic origins depend upon records which were kept by authorities. Various minor outbreaks had occurred in different countries around the world, but were generally not particularly different to seasonal influenza.
Some countries were able to document the early cases:
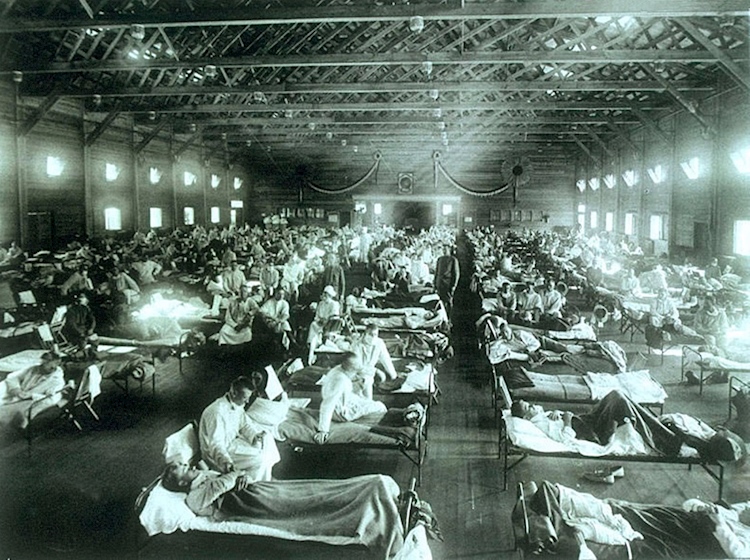
Influenza at the Funston Military Hospital |
The United States of America:
The origins in North America can be traced back to a military camp, Fort Riley, in Funston, Kansas. One of the first officially recognised cases was Albert Gitchel, a cook at this camp, who came down with influenza on 4th March 1918. Within three weeks many thousands of soldiers had caught the disease and 1,100 had required hospitalisation. There were, however, earlier reports of influenza in some of the farmers in Haskell County, Kansas, not too far away. The local doctor, Dr Loring Miner, was so concerned about the severity of this influenza, that he notified the public health officials3 despite the fact that influenza was not a reportable disease. There were no other official reports of influenza at that time in the country. The disease, though severe and rapid, left the district as quickly as it came. |
Some of the Haskell County farmers joined the recruits at Fort Riley. There is the possibility that they had introduced the disease to the camp4. Others have theorized that the disease had been brought in by Chinese contract workers at the camp4. There had been periodic epidemics involving Indo-Chinese soldiers fighting in Europe between 1916 and 1918 (called the Annamite pneumonia)4. From Fort Riley the disease appears to have rapidly spread to other military camps in the USA. By the end of April there were outbreaks in 24 of the 36 military camps. The disease was taken over to Europe with the American troops2a. The influenza decimated the US troops while they were in Europe. Measures within the USA to prevent the spread included the banning of public gatherings (including church meetings), closing schools and cinemas. Masks were supplied by the health departments. Funerals were restricted to 15 minutes and flexible working hours were introduced to avoid crowding on trains. Handshaking was outlawed in some areas.
France:
Influenza appeared in Brest in April 1918. This was the site where most of the American troops disembarked. The disease spread in three waves from April throughout the country and particularly affected the armies, perhaps because of their crowded conditions. The initial wave of influenza in spring of 1918 affected many but there were few deaths. "La grippe", affected 39,559 people in the French army in the three months of May/June/July with a total of 37 deaths5.
There was an outbreak of "purulent bronchitis", which occurred in a British military camp in Étaples on the northern French coast in late 1917. Some suspect that this was an early outbreak of influenza. The outbreak was reported in the Lancet in July 19186. Some authors consider this to be the beginning of the pandemic, but the description given in the article does not describe the typical influenza-like-illness occurring before the symptoms of pneumonia, raising the question of whether this was, in fact, the same disease.
Records relating to the influenza epidemic in France are incomplete. The loss of life in France has been estimated to have been, for civilians, between 125,000 and 250,000 and for soldiers 30,0007.
In 1918 there was significant railway traffic of Spanish and Portuguese workers between France and Spain. |

US Army Camp Hospital No. 5 at Aix-les-Bains, France
Influenza Ward 1 |
Spain8:
Influenza began in Spain in May 1918. It was initially reported as being mild. The third week of May saw the Fiesta de San Isidro, one of Spain's annual holidays. Many people congregated to celebrate and consequently spread the influenza rapidly throughout the country. The Spaniards thought that this illness had come from war-torn France and in fact called it the "French Flu". There was an initial phase of this epidemic which lasted about two months. Mortality rates were from 0.04 and 0.65 deaths per 1,000 of the population. The second wave appeared in September 1918 in many parts of Spain. This was more severe and mortality rates were 0.5 to 14 deaths per 1,000 people. Again, national holidays and celebrations caused further spread. |
 Graph from Erkoreka, 20105 Graph from Erkoreka, 20105 |
Schools and universities closed but many other public gatherings continued. In some towns mass church gatherings occurred. The Catholic Bishop declared that the epidemic was a punishment from God and called the people to repentance. The large cathedral masses only served to spread the illness further. Some towns eg Burgos and Zamora, saw mortality figures of 12.1% and 10.1% respectively.
A third wave hit Spain From January to June in 1919. This was not as lethal as the second wave.
The deaths attributed to the influenza were as follows:
- 1918 - 147,114
- 1919 - 21,235
- 1920 - 17,825
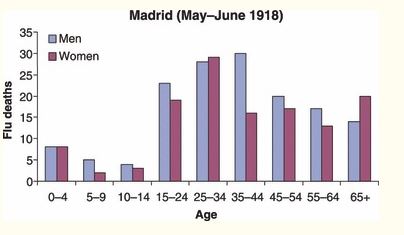
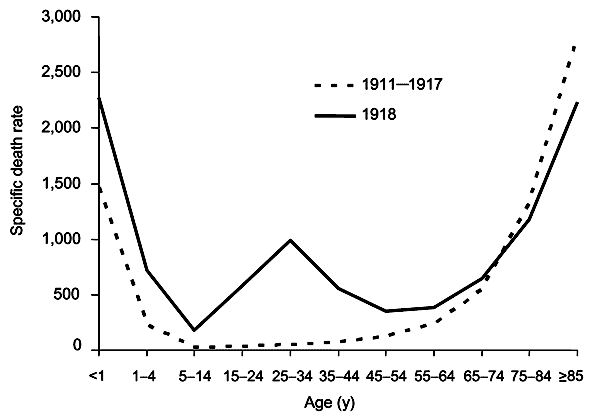
The age mortality profile showed that half of the deaths occurred in the 15 to 44 year old age group, a characteristic of the Spanish flu5.
The United Kingdom:
An early outbreak of influenza had occurred at a military base at Aldershot, England in 1917. It was described as "purulent bronchitis " and many of the soldiers who did poorly were described as having exhibited "heliotrope cyanosis ". It is hard to know whether this was Spanish flu or not.
About half of the doctors from England were with the troops in France, with most of the older doctors (perhaps not as up-to-date) left at home. This became a problem when the influenza numbers became high.
England was used to censorship in the press throughout the war. The public were not informed about the influenza pandemic until May 1918, when it was diagnosed in Glasgow. By June it had hit London: the weekly deaths rose to a peak of 287 at the fourth week9. As with many other countries this first wave seemed relatively benign. The disease was described in the British Medical Journal in July 1918 as a three day illness with full recovery after five days10. The Local Government Board, the government body most responsible for making recommendations, made no attempt to investigate. Sir Arthur Newsholme, the chair of the Local Government Board stated "I have little hope of success of any personal or public measures against influenza which will not influence even more favourably the incidence of bronchitis and pneumonia."9.
The second wave hit in October was severe. In London the weekly death rate surged to a peak of 2,458 in the fourth week, with almost as many in the fifth9. Despite knowing the effects that this influenza had had on other countries, England was slow to act. Newsholme later commented that "I did in my official capacity prepare in July last a memorandum for public use, but on the balance of considerations its distribution was not considered expedient at that time. There are national circumstances in which the major duty is to 'carry on' even when risk to health and life is involved.". The matter was not brought before parliament until October 1918 and even then no significant national strategy was formulated.
|
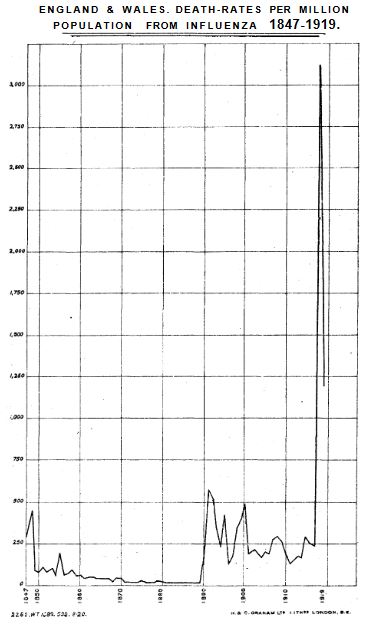
Mortality Figures for England
1847 to 191911 |
Mortality Figures for the United Kingdom, 1918–1919
showing the three phases of the disease
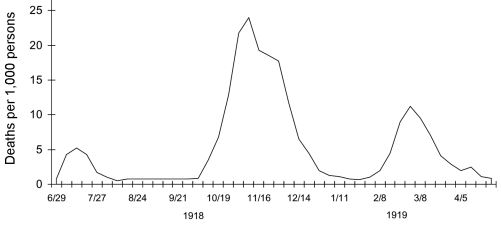
Taubenberger and Morens 200612 |
Efforts were locally managed and not co-ordinated. Some general advice was given such as avoiding crowds, wearing extra layers, not shaking hands, not kissing. Efforts were put in to disinfect and fumigate.
The Spanish Flu was responsible for causing 228,000 deaths in England by the end of 1919.
At the end of 1919 the English government was strongly criticized in the press for its inaction in terms of public health measures to deal with this pandemic.
|
South Africa:
At the time, South Africa had a population of 6,115,212. By November 1918, the number of people who had died from influenza totalled 139,471, giving a mortality rate of 22.8 per thousand13.
New Zealand and the Pacific Islands:
The estimated population of New Zealand in 1917 was 1,160,188. Thirty three percent of the population was infected by the Spanish flu. In the three months from October to December 5,471 people died.
A small trading steamer, the Talune, left New Zealand in October and sailed with cases of influenza on board. The islands that it visited had no maritime quarantine. It visited Fiji, Tonga and Samoa and the Spanish flu rapidly infected each population. All of the native population of Fiji came down with the disease. Seven percent of the Tongan population died as did twenty percent of the Samoan population. The Australian light cruiser HMAS Encounter was dispatched on 24 November 1918 to provide medical assistance to all three islands, with teams disembarking on Samoa and Tonga to combat the disease14.
Clinical Features:
Clinicians overseas noted that there were different presentations of this influenza. The form least likely to cause death was the most common in the first wave of the pandemic, which started in June 1918. This form consisted of a sudden severe illness characterised by high fevers and weakness leading to prostration for three days, then recovery. Dr Herbert French MD FRCP (physician to the royal household and to Guy's hospital) saw thousands of these cases and described the milder form as follows:
| |
"The men's temperatures were generally about 1030F or 1040F; the pulse rates were less raised in proportion; the tongue was coated; the face flushed; the eyelids a little drooped as though the patient were but half awake; in in a very considerable proportion of these cases, either at the very beginning or within a few hours of the onset, there was huskiness of the voice and a tendency to hawking and throat-clearing, less often to actual cough. The throat was complained of as being sore so that it was difficult to swallow or to speak; frothy expectoration, not large in amount, was brought up rather from the mouth and pharynx and larynx than from the bronchial tubes. There was a varying degree of bright reddening of the posterior part of the palate, uvula, fauces and pharynx without white spots or folliculi of pus; without exudation and often without swelling of the tonsils or cervical glands. In some, on the contrary, the tonsils, besides being reddened, looked swollen and enlarged and there might be tenderness on either side of the upper part of the neck below and behind the angle of the jaw, suggesting that the lymphatic glands were inflamed, too, though palpable glandular enlargement was not as a rule a feature of these cases. Headache, especially of the type in which the head does not ache so much when it is kept still, but aches badly when there is a change in posture such as when the head is rolled from side to side or some effort od coughing is made, was prevalent in many cases."15 |
This form of illness was given the nickname "three-day influenza". No specific treatment was needed. Patients were treated with bed rest and none of the drugs available at the time (aspirin, salycilates or quinine) changed the course of the illness. One feature was the rapidity of spread. Within days, large numbers of people were infected.
Lifting of restrictions may have allowed the second wave to occur. The second form of the disease was more apparent in the following autumn and winter. The dominant form of influenza was still the "three-day influenza".
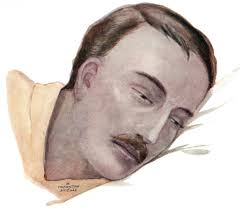
Heliotrope cyanosis |
The second form was often called "pneumonic influenza". About one in five developed this later type, characterised by purulent pneumonia and "heliotrope cyanosis". The course of illness might start the same way as with the milder form. Whereas in the milder form most patients would start to recover after three days, in the second form the patient would suddenly worsen and be dead in 24 to 48 hours. The symptoms were typically chest pain, cough and dyspnoea. Tachypnoea would be quite apparent. Heliotrope cyanosis was seen as an ominous sign. This was cyanosis of varying hues seen over the face and/or ears. Its presence did not always correlate with dyspnoea, fever or other symptoms, but few people who developed the sign ever survived. |
Other physical signs suggested lobar pneumonia; "dullness, bronchial breathing, bronchophony, pectoriloquy and crackling rales over part or whole of one lobe"16. French, however, points out that lobar pneumonia on post-mortem was uncommon, but described the observed findings as "a conglomeration of changes which included bronchitis, and peribronchitis, coagulative oedema, haemorrhage, collapse, broncho-pneumonia, abscess formation, and compression by pleuritic effusion, totally different to anything ordinarily seen in the post-mortem room"16. He also described an albuminous exudate between the alveoli and the capillaries seen by microscopic examination of post-mortem lung tissue. It would appear that he was describing what we now call adult respiratory distress syndrome (ARDS). A few patients did not start with a typical influenza-like illness but presented with a pneumonic illness at the onset, begging the question of whether in these circumstances these patients had bacterial pneumonia de novo as opposed to being secondary to influenza.
| The Spanish Flu was different to other influenza epidemics in that it caused significant mortality in young, fit people, i.e. in the 14 to 40-year-old age group. This was in contrast to the usual pattern of the highest mortality in the very young and the very old. It has been argued that this characteristic might have also been a feature of the situation at the time. Hundreds of thousands of soldiers in this age group were crowded in poor conditions at the battlefront, on ships and in hospitals. This increased the likelihood of spread but also increased the likelihood of secondary infection: secondary bacterial pneumonia being the most common cause of death. However, this pattern of mortality in the young appears to have been present in most of the countries, not just those directly involved in war. |
 |
The Spanish Flu in Australia
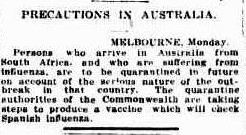
Australia was in a good position to prevent the pandemic affecting the population. The government knew of the spread around the world and the Commonwealth Quarantine Service had been informed in July of 1918 of an impending epidemic of a "severe form of influenza"17. Despite censorship the public were aware to some degree through the newspapers. These had published updates over the months from June to October 1918, documenting the spread to countries such as England18, Europe19, South Africa20, 21 and the USA229, 23. Capetown in South Africa was of particular importance because of the ships calling in there on there way back from Europe as they returned the soldiers at the end of the war. The newspaper articles were typically small and factual and had not sensationalised the issue. In mid-October 1918 cables (telegrams) were received from New Zealand and South Africa, warning of the pandemic:
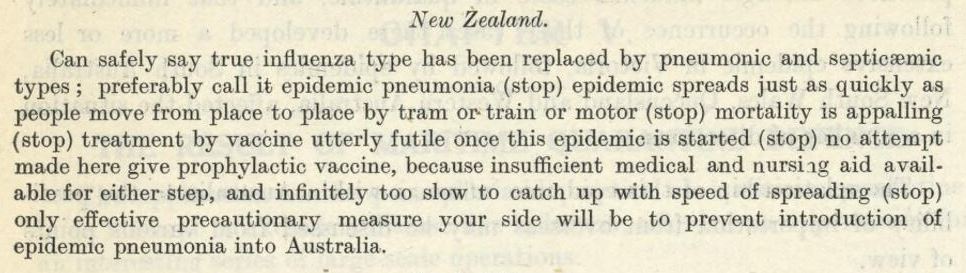
A telegram from the New Zealand Government24 |
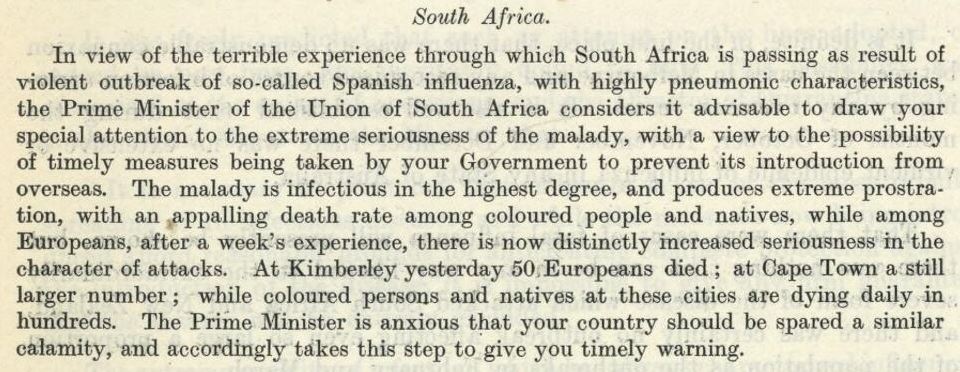
A telegram from the South Africa Government24 |
Australia, being isolated by nature of its circumference of large oceans, had an advantage: travel from most countries enabled sufficient time to determine if influenza was on board any ship. The exceptions were travel from New Zealand and the north. As travel to and from Australia was only by ship, Australia only had to shut down its ports, which it did on 17th October 1918. This was just in time as the first ship with influenza, the SS Mataram, arrived in Darwin from Singapore the next day. Another ship, the Chiron, arrived with influenza in Broome, W.A. from Singapore25. Another ship, arriving in Sydney from New Zealand on 25th October, had patients with influenza and was successfully quarantined at the North Head Quarantine station. In December, the HMAT Boonah, having left England in October 2018, arrived in Western Australia with over 300 sick men in board. The ship was quarantined at Woodman Park where the soldiers disembarked. Twenty seven soldiers died as well as four medical staff. The Australian Quarantine Service intercepted 323 vessels over the first 6 months of the quarantine: 173 of these had influenza on board. Infected passengers were quarantined until fully recovered. The service checked 81,510 people and identified 1,102 infected with influenza26.
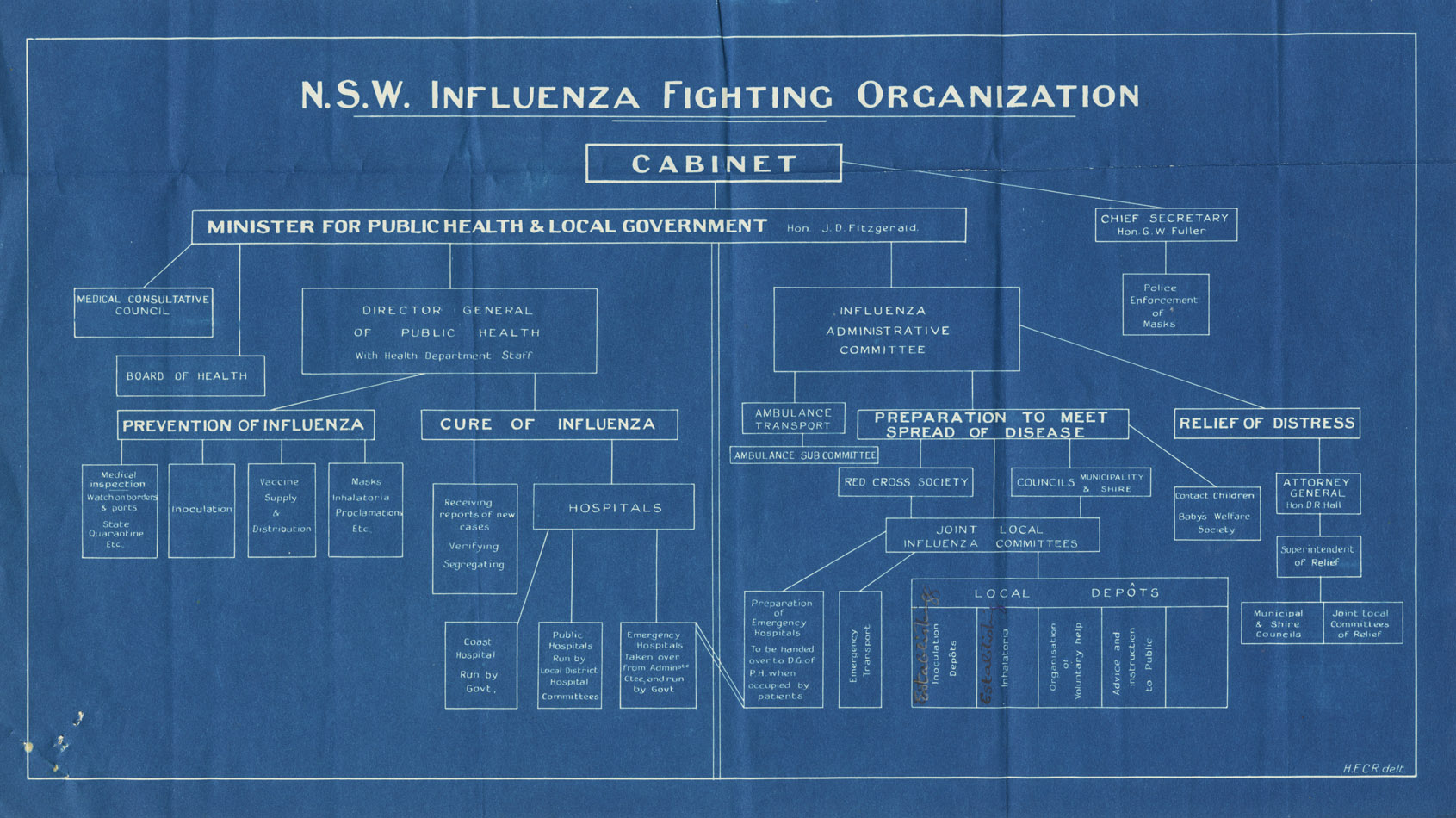
On 26th and 27th November 1918 the Australian Government held a national influenza planning conference in Melbourne. Present were the state Ministers of Public Health, the director generals of each state health department and the presidents of the state British Medical Association (the AMA did not begin until 1962). At the conference it was determined that each state would organise, as required:
- maritime quarantine
- land quarantine, including transport restrictions
- the declaration to the Commonwealth Quarantine Service of any case of pneumonic influenza
- emergency hospitals
- vaccinations
- ambulance services
- medical staff
- public health campaigns
|
×
![]()
NSW Influenza Organizational Management
NSW State Archives & Records
Click to enlarge
|
And that upon the declaration of a state being infected that
- interstate land and maritime transport (except goods and mail) would cease
- all public meetings would cease including schools, church meetings, cinemas, music halls, race meetings
- military camps would be disbanded
- the Commonwealth would make military medical and nursing staff available
Further recommendations included:
- the formation of state advisory committees consisting of each state Chief Health Officer and a limited number of members from the local British Medical Associations.
- establishing vaccine depôts
- the establishment of special hospitals
- organising medical and nursing assistance
- issuing advice to local authorities
- supplying the public with respirators (masks)
- that each state had to come up with a contingency plan to cope with greater numbers should these services be overwhelmed.
Whilst this represented good early planning by allowing each state to have individual control, the Government had lost an opportunity for a well-co-ordinanated approach. Later differences in management and bickering between states reduced the effectiveness of the campaign. Cumpston was critical of the lack of co-ordination amongst the states11a.
The following quarantine stations were used to quarantine incoming passengers in 1919:
- North Head in Sydney, New South Wales
- Lytton in Brisbane
- Point Nepean in Victoria
- Bruny Island in Tasmania
- Woodman Point in Western Australia
- Torrens Island in South Australia
- Channel Island near Darwin in the Northern Territory
In 1919 there were significant numbers of soldiers returning from the war. Many of the naval ships, whilst still in the northern hemisphere, had to deal with the Spanish Flu. These included the destroyer HMAS Huon, the battleship HMAS Australia, HMAS Melbourne, HMAS Sydney, the Torrens and the HMAS Brisbane. The HMAS Brisbane had 183 of her crew of 400 become infected: three died. The troop carrier HMAT Barambah was heavily affected with half of the people on board coming down with influenza, twenty died (this included four of the nurses).
The Royal Australia Navy provided a former patrol vessel, the HMAS Sleuth, to monitor each ship coming into the North Head Quarantine Station in Sydney, to ensure no soldier jumped ship. The Sleuth was attached to the training ship HMAS Tingira, which was moored in Rose Bay14. In February approximately 1,000 soldiers fled the North Head Quarantine Station when they became aware it was infested with snakes. They were marched through Sydney and made to camp on the Sydney Cricket Ground for four days to fulfill quarantine27.
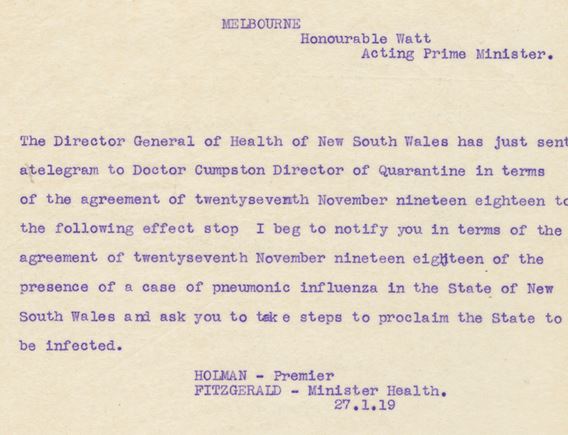
It was only a matter of time that someone, having caught the disease whilst in quarantine, would be released while still asymptomatic. The Commonwealth Quarantine Service had predicted that there was a reasonable chance that the national quarantine would fail at some point27. The first cases of Spanish flu appeared in Melbourne on 9th January 1919. These cases were not notified to state authorities. It must be remembered that cases of influenza-like illnesses were a regular occurrence around Australia. Diagnosing Spanish flu rather than the usual influenza was difficult because the first cases were mild. The Commonwealth Quarantine Service had foreseen this difficulty and had defined influenza as "Influenza, or any febrile, toxic, septicaemic condition similar to influenza, is hereby declared to be a quarantinable disease"17. This definition prevented early containment because it meant that the first patient had to be very sick before notification was made. With high infectivity and a short incubation period (two days), the influenza had already spread before the first patient became sick enough to meet the definition. By 20th January, 50 to 100 cases had occurred and it was apparent that this was a severe form of influenza. But even by 24th January, no declaration by the Commonwealth had been made despite numerous deaths, the culturing of B. influenza and 14 patients per day being admitted to the Melbourne Hospital. The reason, according to Dr McMeekin, the superintendent, was that "they had not met with the serious types"29. The decision not to declare this was made in joint discussions with Dr Cumpston (Director of the Commonwealth Quarantine Service), Dr Robertson (Chairman of the Board of Health, Victoria), Dr Mitchell (quarantine officer, Sydney), Dr Penfold (chief quarantine officer in charge of the CSL) and Dr McMeekin. The various states were none-the-less advised of the situation29. The Spanish flu was fully established in Melbourne by 31st January. The outbreak in Melbourne rapidly spread to South Australia, New South Wales and Queensland, demonstrating that border quarantine in Victoria was not instituted early enough. The outbreak in Sydney was fully established by March 1919. South Australia, probably by virtue of a later, strict quarantine, managed to control the outbreak.
| This delay in notification allowed the disease to spread to NSW. On 24th January 1919, "S. L.", a soldier at the No. 4 Military Hospital at Randwick was reported to have an illness consistent with influenza. He had travelled from Melbourne on 21st November, on a train alongside a civilian who was clearly unwell. Within two days of being at the hospital this soldier had given it to four nurses. By that time seven other soldiers from the same train had come down with the disease. NSW was officially declared to have the disease on 27th (NSW Government Gazette) and 28th January (Commonwealth Government Gazette) under the Quarantine Act30. |
 |
Victoria followed suit with an official declaration the next day. In the week ending 1st February, there had been 23 cases diagnosed in NSW. All had either caught the disease in Melbourne or had caught the disease from someone else who had caught it in Melbourne.
NSW closed the interstate roads. However, it allowed ships to arrive on the proviso that no ship arriving from Victoria should have physical communication with land in NSW until 96 hours had passed since departure. This arrangement was decided without discussion with the Commonwealth Quarantine Service. Queensland also varied the terms of the November agreement by letting people living within 10 miles of the border to cross the border. Western Australia put the transcontinental train under quarantine despite the fact that the train had left Victoria before the quarantine had been announced.
Because the various states were not acting in agreement with the November agreement, the Commonwealth Government temporarily withdrew its support. The states varied their arrangements for a while, but finally settled on the following:
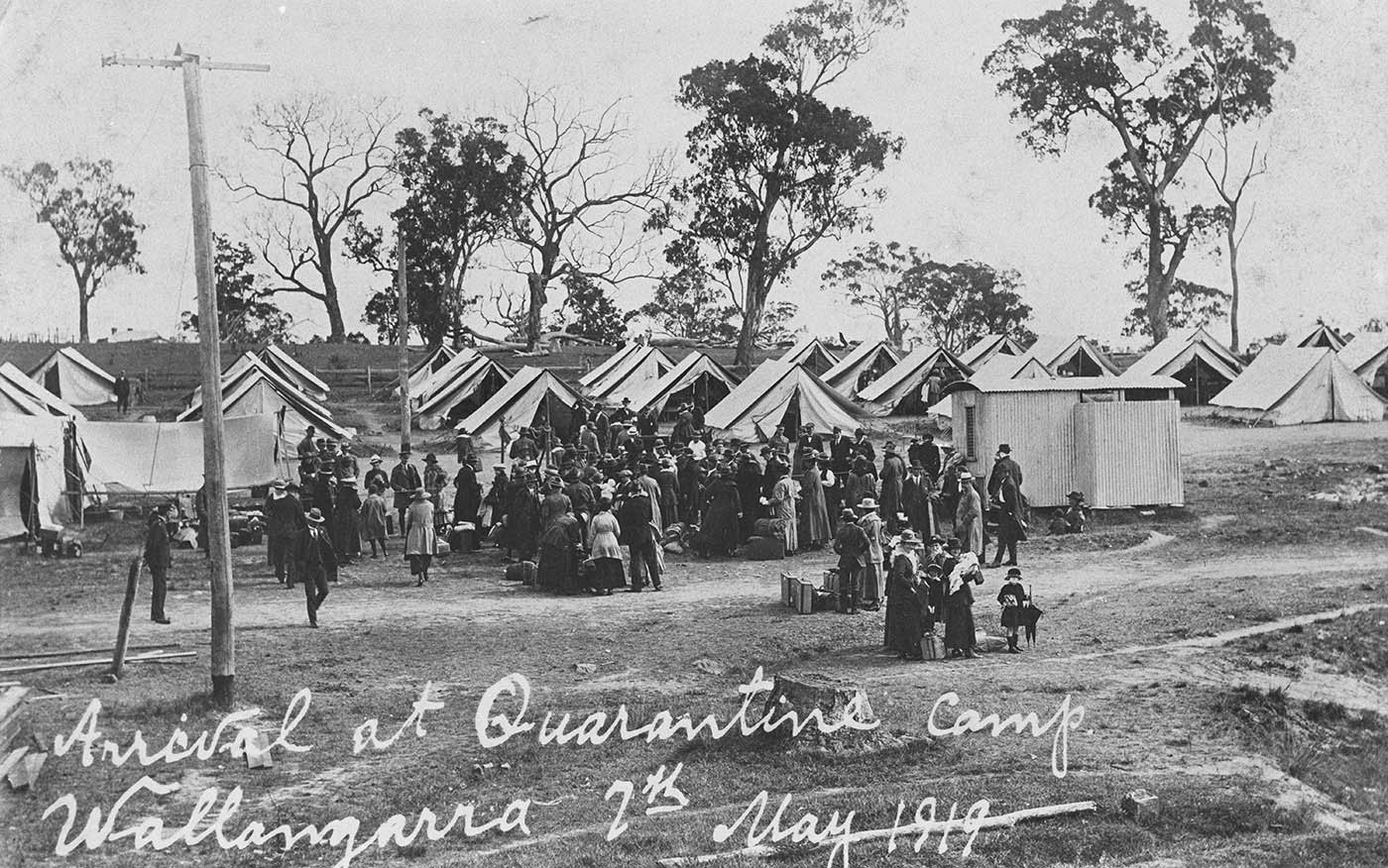 |
- QLD - a quarantine station was set up at Wallangarra (a tent town), enabling people to pass between NSW and Queensland once they had been quarantined for seven days.
- NSW - entry was permitted at one or two locations given a quarantine period of four days. Ocean vessels could enter after a four day quarantine.
- VIC - had no restrictions.
- SA - initially allowed for a seven day quarantine period but no quarantine tents were ever set up so SA had an absolute blockade between itself an Victoria. Maritime quarantine was managed by the Commonwealth.
- WA - no interstate land travel, maritime entry only after seven days quarantine.
- TAS - required a seven day quarantine for any ship.
|
These arrangements persisted until the movement of persons was administered by the Commonwealth in stages between February and May 1919. The concept of quarantine was good, but the practice was not. Many breaches occurred particularly between NSW and Victoria, where the crossing points were too many to be managed effectively. As well, the quarantine camps at the borders did not entail the daily medical or even daily temperature checks, in contrast to maritime quarantine. For the whole time of operation in NSW and Queensland, not a single person with influenza was discovered at the land quarantine stations, obviating the question of the value of interstate quarantine. South Australia, with fewer roads crossing the borders, managed a much more successful quarantine. Note that South Australia's mortality statistics did not rise above the normally observed values.
NSW declared the compulsory wearing of masks on 31st January for anyone in Sydney traveling on a train, tram or in a public place or an office or a shop frequented by the public. Many of the requirements were relaxed by the 28th March.
Train travel out of Sydney from 4th April, however, required
- a signed declaration stating that the person had not had contact with anyone with pneumonic influenza within the previous two days
- vaccination within the prior 3 months
- a medical certificate dated within 24 hours of travel to say that they had no evidence of the disease
- to have had a zinc sulphate inhalation within 24 hours of the proposed travel
Medical clinics were set up at various locations around Sydney to provide the travel fitness certificates free of charge. These conditions remained until 8th July.
NSW provided free vaccinations against influenza in public clinics from 27th November 1918 until 17th May 1919. The vaccine was also made available to private practitioners. Very many people presented for inoculation. Over 800,000 doses were administered in NSW with an average of two inoculations per person, meaning that almost one quarter of the NSW population was inoculated. At the peak, the Hyde Park Recruiting Depot administered 9,731 doses in one day alone! Side effects were mild and infrequent, at most a mild fever and some aches. Some people found that it reduced the symptoms of their rheumatism or chronic catarrh and so they presented every two to three weeks to get continued relief31. From the figures collected in NSW hospitals, those who had not been inoculated and came down with the disease, had an 8.3% mortality rate vs those who had been inoculated at least once, who had a 1.1% chance of dying31.
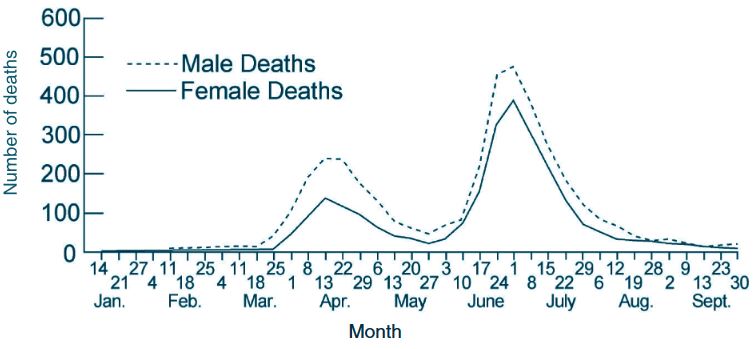
NSW saw two waves of Spanish flu: both lasted about 10 weeks. From the 19th March to 27th May, 1,892 deaths were recorded in NSW. In the second wave from 28th May until 25th August, 3,899 deaths were recorded. There were two occasions, lasting a fortnight each, where there were insufficient hospital beds to manage the severely ill. The first of these was from 8th to 18th April. The second peak was at the end of June. The government had provided 2,500 metropolitan hospital beds but one hospital of 500 beds (created on Randwick Racecourse) could not be opened because of a shortage of doctors and nurses: many of them were still overseas because of the war. Fifth year medical students from Sydney University were asked to work32 and the majority volunteered. Retired medical professionals also volunteered and returned to work. It was estimated that 290,000 people in Sydney came down with the Spanish flu (36.6% of the population). The overall case mortality rate was 1.3%33.
"It was a dreadful time. Very short of doctors. Emergency hospitals everywhere - the Deaf and Dumb Institute, the Showground. I hadn't been in a hospital yet. I couldn't take a temperature but they showed you what to do. We went out on rounds to the people. I suppose we looked like doctors. The doctors were so busy. A lot still hadn't come back from the War so they had to use us. I worked from a Depot in Flinders Street, Darlinghurst, a church there, then from Woolloomooloo, down the Stanley and Palmer Street brothels - I was only 19. You'd go into these houses and there'd be no-one up and about and they had no food. Volunteers used to come with food but they couldn't keep up with it. I got the flu myself but not badly. I went home and to the local doctor. We were never vaccinated that I remember".
(from interview with Dr Cawley Madden, 8 March, 1979. Held in Sydney University Archives) |
As with observations overseas the Spanish flu in Australia was more likely to have severely affected young adults. Whereas it is often thought that this fact was due, particularly with regard to the troops fighting the war, to unhygienic, crowded conditions, this was not the situation in NSW at the time, suggesting that this propensity to kill young people was related to some intrinsic characteristic of this particular strain of virus. What was also observed was that pregnant women fared even worse. Of 224 pregnant women admitted to Sydney hospitals, 60 died, that is almost 27%. Of the women who had been vaccinated only 9.5% died. Forty six women had premature deliveries (6th to 8th month). Of these 48% of the women died34.
It might be noted that pneumonic influenza was made a compulsorily notifiable disease at the November conference and under section 8 of the Public Health Act, however it proved that the definition was too narrow. This meant that many or most cases of influenza were not being reported so the medical profession was asked to report all cases. This was done through the sending of a circular and via the press.
| The press was also used to ask people who had symptoms to notify the authorities. They would then be visited by one of the departmental medical officers and sent to hospital (forcibly if needed) if they had the disease. Remaining members in the house would then be quarantined and visited daily. They were also offered zinc inhalations. These measures were initially employed but once the local epidemic had progressed, they were relaxed.
Another way to notify the authorities was to hang a sign at the window. This had "SOS" in large figures. |
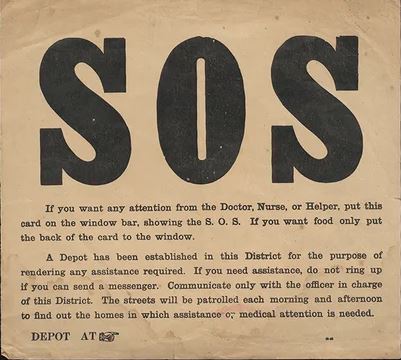
from the National Library of Australia
|
From Sydney the Spanish flu spread into the rest of NSW. The severity in the country was generally less than in the city and the deaths fewer. Mortality rates in the country were estimated to be 2.3 per 1,000 population vs the Sydney figure of 4.3535.
South Australian mortality figures were so low that there was no apparent increase over normal seasonal rates. It is likely that the strict quarantine measures accounted for this despite the initial influx of cases from Victoria.
Tasmania implemented a strict maritime quarantine with a 14 day quarantine period, later reduced to 7. They were required to reduce it again, but in April 1919 they defied the Prime Minister by refusing to reduce it, arguing that their quarantine had kept Tasmania free of the disease - the only cases being those who had arrived by boat and who had been successfully managed under quarantine. In response to their refusal, the Prime Minister threatened to divert shipping away from Tasmania. The effect of this would have been to deprive Tasmanians of wheat (and hence flour) as well as other goods and stop the export of fruit and vegetables which were in danger of rotting on the warves36. Tasmania had lost its main income (tourism) and was suffering as a result. Tasmania threatened to secede from the newly formed Federation37. As a result of keeping to its resolutions, Tasmania escaped with the lowest recorded mortality rate recorded in the world.
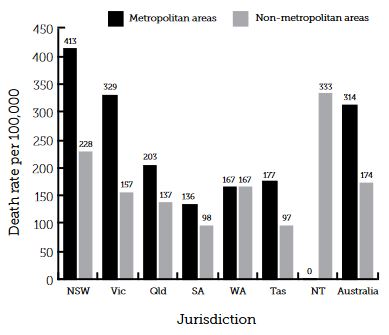
Comparative mortality figures (Kaiko, 2015)38 |
Total deaths by state:
- NSW - 6,244 deaths
- WA - 638 deaths
- SA - 532 deaths
- Qld - 830 deaths
- Tas - 171 deaths
|
Mortality Figures for Australia (from NSW Public Health Bulletin39)
|
Public health measures:
| Quarantine services had been a state responsibility. However, with the formation of the Federation in 1901 some services were seen to be better handled by the new Commonwealth Government. In 1909 the Commonwealth Quarantine Service had been set up40 and by 1913 the government transferred state quarantine services to a national service with the formation of the Commonwealth Quarantine Service41. Its chief officer reported to a Director responsible to the Minister for Trade and Customs under the Constitution [Section 51 (ix)]. Dr John Howard Lidgett Cumpston (1880 to 1954) had been appointed the Director of Quarantine in this period. |
 |
Quarantine was the first and most effective measure that was taken to prevent significant spread of this disease and subsequent mortality. Various other measures were taken:
- isolation of infected people
- making influenza a notifiable disease. This was rescinded on 8/8/1919 as it no longer served a useful purpose.
- banning of group meetings e.g., schools, theatres, church meetings, pubs, race meetings
- planning to provide extra hospital beds
- the closure of country schools so that they could be used as hospitals
- spraying of streets
- requiring the wearing masks in public in some areas. Penalties of heavy fines or potential imprisonment were administered to defaulters42
- provision of medical and nursing care to those sick at home
- distributing assistance to affected households in the form of food, drugs and where needed, money
- freeing up of the ambulance service for influenza work
- providing extra hospital beds
- restriction of public transport
- establishing quarantine camps at state borders.
- encouragement of personal measures e.g. cough hygiene, hand washing
- establishment of inhalation stations
- public education
- arranging relief depôts around the country, staffed by medical, nursing, clerical personnel and volunteer assistants.
- the sending of circulars to doctors to inform them about the symptoms of pneumonic influenza, its prevention, its treatment, about the use of respirators and about establishing inoculation depôts.
- the establishment of the Consultative Council43 of the British Medical Association, which gave medical advice to the Minister and Public Health
- the establishment of the Metropolitan Influenza Administrative Committee and the Country Influenza Board.
- recruiting volunteer services e.g. the Red Cross to assist with nursing and other activities
- liaising with manufacturers of masks to increase production before the need arose and the public were required to wear them
|

Sydney Morning Herald, 3/2/1919 p. 5
|
In NSW relief depôts were established to assist people who came down with the Spanish flu. The depôts helped co-ordinate evacuation to hospital of those who were sick. They provided nursing care for whole households that became sick together, or who otherwise needed help. They saw to the administration of financial relief when needed. These depôts also made arrangements for children who lost (either temporarily or permanently) their parents/carers. The medical officers in most of the Sydney depôts, of which there were about 100 in Sydney, were often fifth year medical students. The depôts had nurses and were usually also assisted by Red Cross volunteers.
Admissions to influenza hospitals were controlled by Public Health.
As an example of the provision of extra hospital beds, Sydney made arrangements to use:
- 200 beds at the Coast Hospital
- beds at the public and private hospitals
- the publicly controlled convalescent hospitals at Denistone House (Eastwood), Carrara (Rose Bay), Grayclifffe Hospital for Babies (Vaucluse)
- the Deaf and Dumb and Blind Institute (City Road)
- the Walker Convalescent Hospital
- the Balmain Drill Hall
- Balmain Kindergarten
- the skating rink at Moore Park
- the grandstand at Randwick Racecourse
In Sydney, numerous inhalatoria were set up to provide the public with zinc sulphate inhalations. A number of tramcars were fitted with equipment to nebulise zinc sulphate within the enclosed tramcars to provide mobile inhalatoria.
Public response:
It is hard to gauge public response because of variability. The Spanish flu brought out the best in some people and the worst in others. There were many volunteers, eg the Red Cross Service, who put their lives at risk in order to help others. Nurses and doctors continued to work despite putting themselves into high risk situations. Most of the fifth-year medical students at Sydney university volunteered to work in medical positions, particularly in the relief depôts. However, some people refused to help their neighbours in need for fear of catching the disease themselves.
Cumpston thought that the media had sensationalised the pandemic, leading to panic. This was not helped by the press comparing the Spanish flu to the Black Death of medieval times.
Most people complied with wearing masks in public. Some, who did not concern themselves with the risk that they generated for others by refusing to wear masks, were fined.
Some dockyard workers refused to unload ships. Other services were reduced because of workers being sick.
Perhaps because the medical profession was not able to offer an effective treatment, many alternative treatments were offered in the media, preying on people's fears and offering them worthless remedies.
Medical Management
Prevention:
In 1919 it was thought that influenza was caused by a bacterial infection. Haemophilus influenzae had first been described in biopsies by the Polish microbiologist Bujwid Odo Feliks Kazimierz (1857 to 1942). Richard Pfeiffer (1858 to 1945) had discovered this bacterium in patients in the 1889 to 1892 influenza epidemic. It was thereafter names "Pfeiffer's bacillus", or sometimes referred to as Bacillus influenzae. Not all of the medical world was convinced that this was the cause of influenza as it had not satisfied all of Koch's postulates. The fact that the causative agent for influenza was not filtered out with the normal bacterial filters, had not been published at the beginning of the pandemic. Various other bacterial organisms had also been isolated from those who developed influenza pneumonia. These included Pneumoccocus, Steptococcus and Micrococcus catarrhalis (Moraxella catarrhalis). Viruses were not discovered until 1933. Because there were no antibiotics at this time, secondary pneumonia was commonly fatal.
Zinc sulphate inhalations:
Zinc sulphate/steam inhalations were commonly used as a preventative measure ealy in the pandemic, on the basis that the zinc sulphate would kill the bacteria. "Neither the fixed nor the portable spray apparatus appeared to yield results that encouraged their continuance"43 and so the usage faded out.
| As the thinking was that influenza was due to B. influenzae (H. influenzae), efforts were made to disinfect workplaces, hospitals and even public places. Attempts were also made in some places to disinfect the respiratory tract. The photograph opposite shows an inhalatorium employed by Kodak for its workers. An inhalatorium was a place where the employees could come and inhale zinc sulphate in steam to disinfect the respiratory tract. The instructions were to place all of the face in the opening and take 15 slow deep breaths. This was done twice daily. |

An Inhalatorium at Kodak
courtesy of Museums Victoria
|
Masks:
In some areas of Australia, e.g. Sydney, it became a legal requirement to wear a mask when in public. Fines were issued for transgressors. Medical and nursing staff wore gowns and masks when treating patients but commonly became infected with the virus and a number of deaths ensued.
Vaccination:
Vaccinations had been tried overseas. In South Africa, vaccines had been used late in the disease with no benefit44. Australia, however, had two significant advantages. The first was the possibility of delaying the illness through maritime quarantine, the second was that it had a newly established facility for making vaccines. The Commonwealth Serum Laboratories (CSL) had been formed just two years earlier (1916), for the purpose of producing vaccines that were hard to get during the war (tuberculin and smallpox). In 1918 it was commissioned to produce a vaccine against influenza. The CSL managed to produce a vaccine even before the first case of Spanish flu was identified in the country.
The first (test) vaccine was prepared by November 1918. It was made of batches of the following organisms:
| A strain | B strain |
| Organism | Numbers per cc | Numbers per cc |
| M. catarrhalis | 25 million | 125 million |
| Pneumococcus | 10 million | 50 million |
| Streptococcus | 10 million | 50 million |
| G+ve diplococcus | 10 million | 50 million |
The organisms were killed using tricresol (a mixture of ortho, meta and para-cresols). Note that this did not contain B. influenzae as there was no sample available. The vaccine was trialled on 5,155 railway workers in Victoria and compared with 6,247 railway workers not inoculated. Over the study period those not inoculated had an incidence of influenza of 4.03%, Those inoculated once had an incidence of influenza of 4.1%. Those inoculated twice 2.5%. Death numbers were too small to be significant (6 in the uninoculated and two in the twice inoculated groups). Note that this was done in the first phase of the Spanish flu, when the disease had a lesser effect.
It appears that B. influenzae was imported from South Africa (with special permission from the government45) in order to make the final vaccine. It was prepared by December 1918 and consisted of a mix of the following:
| A type | B type |
| Organism | Numbers per cc | Numbers per cc |
| B. influenzae | 25 million | 125 million |
| M. catarrhalis | 25 million | 125 million |
| Pneumococcus | 10 million | 50 million |
| Streptococcus | 10 million | 50 million |
| G+ve diplococcus | 10 million | 50 million |
Multiple strains of the above organisms were employed in manufacturing the vaccine. Some people were given one inoculation and others were given two. It is unclear as to what passage of time separated the two inoculations. The "A" type was given first and the stronger "B" type was given as the second inoculation. One millilitre was given on each occasion. The effectiveness of the vaccine was prospectively studied, which was an important aspect because no extensive work had ever been done on influenza prophylaxis before.
Vaccinations were given by doctors at inoculation depôts, with the public being encouraged to attend. Thousands attended and thousands initially turned themselves away because of the lengths of the queues. Vaccinations were also given by doctors in their private practices46.
Once the vaccine was in usage, the effects were monitored prospectively. The person put in charge of this was Mr T. M. Cherry B.A. The death rate in the uninoculated was 13.8% of those infected and in the innoculated group was 4%. The severity of the disease was also much less in those who received two inoculations. In total the CSL prepared and distributed 3 million doses of the vaccine between 15th October 1918 and 15th March 1919. This was despite the new buildings having been open for only three months and not being of sufficient size for this scale of operation.
Of interest, for the naval expedition to Fiji, Samoa and Tonga, all crew members were vaccinated against influenza at least four times. Not one crew member came down with influenza47.
The Royal Prince Alfred Hospital in Sydney, also produced a vaccine48, which it supplied free of charge. This consisted of the following:
| Organism | Numbers per cc |
| Pneumococcus | 1,000 million |
| B. influenzae | 100 million |
| Streptococcus | 100 million |
| Staph. aureus | 250 million |
| G-ve Micrococcus | 250 million |
The dose was 0.5mls for the first dose and 1.0mls a week later by subcutaneous injection. When supplies ran short the doses were halved.
Treatment:
Isolation:
The patient with influenza was put to bed immediately. This served two purposes. It served to rest the patient who typically felt very lethargic. It also served to isolate the patient from others so as to reduce spread. Some were managed at home, but most were sent to hospital, particularly in Australia. Keeping all infected patients together reduced spread and provided some degree of efficiency in nursing many patients at once. However, when conditions were crowded it would have also increased the spread of bacterial organisms leading to an increased risk of pneumonia.
Symptom relief:
Doctors knew that they had no cure for influenza. Treatment was focussed on symptom relief.
Fever and pain:
Potential treatments included the following analgesic/antipyretics:
- Phenacetin
- Antipyrin (phenozone)
- Aspirin
- Sodium salicylate
- Salol (phenyl salicylate) was used overseas. It had been discovered in 1883. Its use has since been discontinued as it has been found to be too toxic.
Also used was Dover's powder (ipecacuanha powder 10%, powdered opium 10%, lactose 80% by weight. Usual dose from 320 to 640 mg. (5 to 10 grains)).
Various combinations were used, e.g. phenacetin and a salicylate.
Stengel (1911)58 commonly used:
℞.
Ft.
|
Salolis,
Acetphenetidinae........................āā gr. iij:
Pulveris Doveri................................gr. ss. -M.
in capsule No. i.
|
See here for how
to read old prescriptions |
A fever might also be treated with ice packs or cold compresses.
Weakness:
When the patient was seen to be "depressed" (i.e. weak), stimulants were used. These included strychnine, quinine, alcohol and spirits of ammonia. For example quinin 6 to 8 gr per day or small amounts of brandy, whisky or wine.
Catarrhal symptoms:
Conjunctivitis could be treated with boric acid in camphor water with or without adrenalin chlorid or cocain.
Marked coryza:
Runny noses could be treated with an alkaline antiseptic spray such as Dobell's solution (sodium borate, sodium bicarbonate, phenol, and glycerol)or liquor antisepticus alkalinus with or without adrenalin chlorid for nasal congestion or camphor and menthol in vaseline into the nostrils
|
Liquor antisepticus alkalinus59:
Potassium Bicarbonate 600 grains 32.0 Gm., Sodium Benzoate 600 grains 32.0 Gm., Sodium Biborate 310 grains . 8.0 Gm., Thymol 4 grains 0.2 Gm., Eucalyptol 4 minims. 0.2 mls, Oil of Peppermint 4 minims. 0.2 mls, Oil of Wintergreen 7 minims. 0.4 mls, Tincture of Cudbear 300 minims. 16.0 mls, Alcohol (95%) 2^ fluidounces 62.5 mils, Glycerin 10 fluidounces 250.0 mls, Purified Talc 185 grains 10.0 Gm., Water, sufficient quantity to make . . 40 fluidounces 1000 mls |
Cough:
To suppress the cough, options included; ammonium chlorid, sodium benzoate, sodium carbonate with ipecac, senega or squill plus heroin, codein, opium or morphin. Failing this stimulating liniments applied to the back or the chest, flaxseed or kaolin poultices. Sometimes cod liver oil was used.
Nausea and vomiting:
Might be treated with "counter irritants" applied over the stomach e.g. mustard plasters, spice poultices, tincture of iodin or cerium oxalate with trace amounts of cocain hydrochloride and codein or calomel. Failing this subcutaneous morphin or an opium suppository.
Diarrhoea:
Might be treated with bismuth, or chalk with silver nitrate, lead acetate and opium.
Cardiac involvement:
Atropin or belladonna was used to treat bradycardia or other arrhythmias. Tachycardia or low blood pressure might be treated with digitalis. Marked cardiac weakness was treated with ice packs over the heart, strychnine, aromatic spirits of ammonia, moderate alcohol, and/or digitalis.
Other Treatments
Hydrothermal therapy:
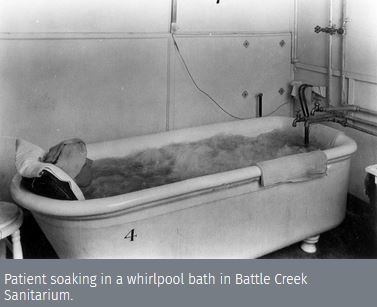
with permission from the
Center for Adventist Research |
Known at the time as hydrotherapy (a term still in use), this was a technique used by Adventist hospitals (sanitaria). The aim was to gently heat the body, using heat packs (fomentations) in conjunction with hot foot baths or submerging the patient in a hot bath until the body reached a temperature of about 390 and then keeping it there for a short period. The head was kept cool using cold packs (see picture). The body was then exposed to brief cooling to cause vasoconstriction in the skin "to lock the heat in". The thinking was to assist the body in its natural response to infection, rather than oppose it by trying to bring the temperature down. There are many modern studies which show that raising the body's temperature mobilizes the immune system, eg Evans (2015)49, Zellner (2002)50 and Evans (2015)51. There is information suggesting that the technique reduced mortality.
The Adventist publication Life & Health Vol. 34 in May 1919, describes the process of using hot fomentations used at the time in detail. Further details can be found in Kellogg (1922)52
|
Fresh air and sunlight:
Because of the high numbers of patients with Spanish flu, many hospitals had to cram patients into available spaces. This, of course, increased the risk of spread of the bacteria which caused pneumonia. There was some evidence from overseas that open tent hospitals and exposure to fresh air and sunlight, improved chances of survivial53.
Quinine:
In 1919 there were very few effective drugs in the pharmacopoeia compared to today. Quinine was normally used for malaria and when successful, brought down the associated high fever. It was tried as a treatment for influenza. Oral administration did not seem to work well. One publication reported success using quinin bisulphate (sic) intravenously in "heroic doses"54 with success.
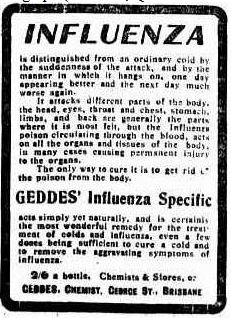
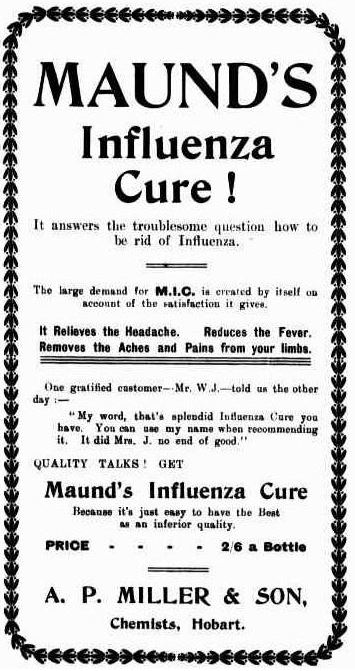
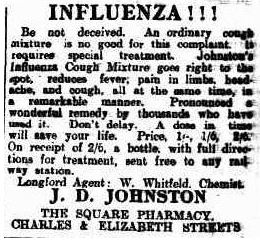
Quackery:
Treatments that did no more than to raise money for the snake oil merchants, appeared in newspapers all over Australia.
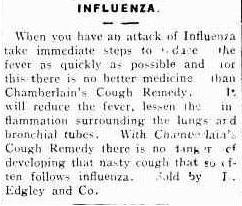
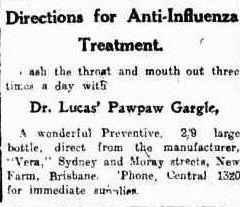
Bathurst Times (NSW : 1909 to 1925), Thursday 2 June 1910, page 1
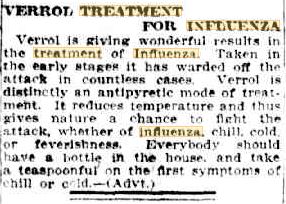
Herald (Melbourne, Vic. : 1861 to 1954), Wednesday 6 August 1919, page 4 |
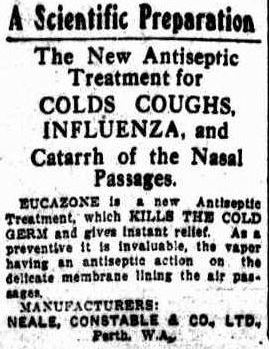
Daily News (Perth, WA : 1882 to 1950), Tuesday 25 May 1915, page 9 |
Telegraph (Brisbane, Qld. : 1872 to 1947), Friday 8 April 1910, page 3 |
Critic (Hobart, Tas. : 1907 to 1924), Saturday 23 September 1911, page 1 |
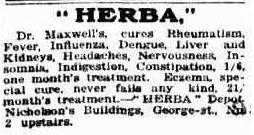
Daily Standard (Brisbane, Qld. : 1912 to 1936), Wednesday 3 September 1913, page 3 |
Daily Telegraph (Launceston, Tas. : 1883 to 1928), Saturday 23 April 1910, page 1 |
Daily Mail (Brisbane, Qld. : 1903 to 1926), Saturday 12 April 1919, page 9 |
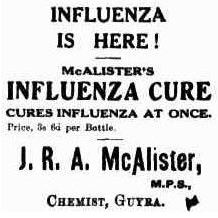
Guyra Argus (NSW : 1902 to 1954), Thursday 3 July 1919, page 2 |
The Outcome of Spanish Flu in Australia
The loss of lives in Australia was terrible, with about 15,000 dying in 1919. The fact that Australia had one of the lowest mortality rates in the world was of some comfort, but the fact that this pandemic killed the majority of its victims in the 15 to 44 year old age group meant that it had a severe impact. This was on top of the 62,000 young lives lost in WW1.
- About 40% of the Australian population developed the Spanish Flu, ie about 2 million Australians were infected.
- about 15,000 died
- about 5,000 marriages lost one partner
- over 5,000 children lost one or both parents
- about 40% of the Sydney population developed the disease: 4,000 died
- 52% of deaths were in the 15 to 39 year old age group
- the mortality rate was approximately 2.7 per thousand of population, one of the lowest in the world
- mortality rate in some Aboriginal communities was nearly 50%55, 30 in some places.
- Australia developed a national Department of Health in 1921 in order to prevent a recurrence of state inco-ordination should the situation ever arise again.
References:
| 1. |
Taubengerger, J.K., et alia, Characterization of the 1918 influenza virus polymerase genes, Nature. 2005 Oct 6;437(7060):889-93. |
| 2. |
Abrahams, A., et al., Influenzo-pneumococcal and influenzo-streptococcal septicaemia - Epidemic influenzal "pneumonia" of highly fatal type and its relation to "purulent bronchitis", The Lancet, 4/1/1919 |
| 3. |
Barry, John, The site of origin of the 1918 influenza pandemic and its public health implications, J. Transl. Med., published online 20/1/2004, doi: 10.1186/1479-5876-2-3 |
| 4. |
Reid, A.H., Origin and evolution of the 1918 "Spanish" influenza virus hemagglutinin gene, Proc Natl Acad Sci U S A. 1999 Feb 16; 96(4): 1651-1656.
|
| 5. |
Erkoreka, A., The Spanish influenza pandemic in occidental Europe (1918–1920) and victim age, Influenza Other Respir Viruses. 2010 Mar; 4(2): 81–89. |
| 6. |
Hammond, J.A.B., et al., Purulent Bronchitis - A case study of cases occurring amongst the British troops at a base in France, The Lancet, 14/7/1917, p.41 |
| 7. |
Guénel, J., Spanish influenza in France 1918-1919, Hist Sci Med., 2004 Apr-Jun;38(2):165-75.
|
| 8. |
Trilla, A., Trilla, G., Daer, C., The 1918 "Spanish Flu" in Spain, Clinical infectious Diseases, Vol. 47, Issue 5, 1/9/2008, p. 668-673
|
| 9. |
Newsholme, A., Discussion on Influenza, Royal Sociaty of Medicine, 1918
|
| 10. |
Botch, O.H., Whittingham, H.E., A Report on the "Influnza" Epidemic of 1918, BMJ, 27/7/1918, p. 82-83
|
| 11. |
Cumston, J.H.L., Influenza and maritime Quarantine in Australia, Commonwealth of Australia Quarantine Service, Service Publication 18, 1919, p. iii
|
| 12. |
Taubenberger, J.K., Morens, D.M., 1918 Influenza: the Mother of All Pandemics, Emerg Infect Dis. 2006 Jan; 12(1): 15–22. doi: 10.3201/eid1201.050979
|
| 13. |
Cumpston, J.H.L., Chapter V, in Reports on Public health no. 4 - Pandemic of 1918-1919, Ministry of health, London, 1920, p.54
|
| 14. |
Swinden, Greg, The Navy and the 1918-19 flu pandemic, The Australian navy institute website, https://navalinstitute.com.au/14244-2/, 5,4,2020, accessed 19/4/2020
|
| 15. |
French, Herbert, The Clinical Features of the Epidemic of 1918-1919, in Reports on Public health no. 4 - Pandemic of 1918-1919, Ministry of Health, London, 1920, p.67
|
| 16. |
Newman, George, Chief Medical Officer's Introduction, in Reports on Public health no. 4 - Pandemic of 1918-1919, Ministry of health, London, 1920, p.67
|
| 17. |
Cumston, J.H.L., Influenza and maritime Quarantine in Australia, Commonwealth of Australia Quarantine Service, Service Publication 18, 1919, p. 7
|
| 18. |
Sydney Morning Herald, Epidemic in London, 26/6/1918, p. 11
|
| 19. |
Sydney Morning Herald, Spanish Influenza, 9/10/1918, p. 11
|
| 20. |
Sydney Morning Herald, Spanish Influenza, 18/10/1918, p. 7
|
| 21. |
Sydney Morning Herald, Spanish Influenza, 5/10/1918, p. 14
|
| 22. |
Sydney Morning Herald, Spanish Influenza, 15/8/1918, p. 7
|
| 23. |
Sydney Morning Herald, Spanish Influenza, 27/9/1918, p. 7
|
| 24. |
Cumpston, J.H.L., Chapter V, in Reports on Public health no. 4 - Pandemic of 1918-1919, Ministry of health, London, 1920, p.54
|
| 25. |
Sydney Morning Herald, Spanish Influenza, 22/10/1918, p. 7
|
| 26. |
Cumston, J.H.L., Influenza and maritime Quarantine in Australia, Commonwealth of Australia Quarantine Service, Service Publication 18, 1919
|
| 27 |
Soldiers in Revolt, The Express and Telegragh (Adelaide), 12/2/1919, p.2
|
| 28. |
Cumpston, J.H.L., Chapter V, in Reports on Public health no. 4 - Pandemic of 1918-1919, Ministry of health, London, 1920, p.52
|
| 29. |
Doctor and Nurses InfectedDaily telegraph, 24/1/1919, p2
|
| 30 |
Commonwealth of Australia Gazette, no. 11, 27/1/1919
|
| 31. |
The members of this council were Dr A.A. Palmer (President), Prof. Welsh, Drs A.E. Mills, Gordon Craig, Sydney Jamieson, D. Thomas, W.F. Litchfield, T.W. Lipscombe, S.A. Smith, Sinclair Gillies, C.H.E. Lawes, A.A.Aspinall and later Drs Harold Ritcie and W.G. Armstrong.
|
| 32. |
Armstrong, W. G., Epidemiology and Administration, in Report on the Influenza epidemic in New South Wales in 1919, 1920 p. 145
|
| 33. |
Armstrong, W. G., Epidemiology and Administration, in Report on the Influenza epidemic in New South Wales in 1919, 1920 p. 144
|
| 34. |
Armstrong, W. G., Epidemiology and Administration, in Report on the Influenza epidemic in New South Wales in 1919, 1920 p. 147
|
| 35. |
Armstrong, W. G., Epidemiology and Administration, in Report on the Influenza epidemic in New South Wales in 1919, 1920 p. 165
|
| 36. |
Tasmania's Position. Decision of the Cabinet. Restrictions must be maintained, The Mercury (Hobart), 9/4/1919, p.7
|
| 37. |
McQueen, H., The "Spanish" Influenza Pandemic in Australia, 1912-19, Australian Society for the Study of Labour History, Canberra, accessed online, 22/4/2020, https://labourhistorycanberra.org/2018/06/the-spanish-influenza-pandemic-in-australia-1912-19/
|
| 38. |
Kako, M., et al.,. Spanish influenza of 1918-19: The extent and spread in South Australia, Australasian Epidemiologist, 22(1) pp. 48-54.
|
| 39. |
Curson, P., McCracken, K., An Australian Perspective of the 1919-1919 Influenza Pandemic, NSW Public Health Bulletin, Vol. 17 n0 7-8, p.104
|
| 40. |
Cumston, J.H.L., The History of Smallpox in Australia, Commonwealth Department of Health, Service Publication 29, 1925
|
| 41 |
Cummins, C. J., A History of Medical Administration in NSW 1788-1973, NSW Health, 2nd Edition, 2003
|
| 42. |
Mask prosecutions, Sydney Morning Herald, 25/2/1919, p7
|
| 43. |
Armstrong, W. G., Epidemiology and Administration, in Report on the Influenza epidemic in New South Wales in 1919, 1920 p. 164
|
| 44. |
Sydney Morning Herald, 22/10/1918, p. 7
|
| 45. |
Sydney Morning Herald, Spanish Influenza, 24/10/1918, p. 6
|
| 46. |
Inoculation, Sydney Morning Herald, 21/1/1919, p11
|
| 47. |
The Case for InoculationDaily Examiner, 23/4/1919, p1
|
| 48. |
Supplies of VaccineSunday Times, 9/2/1919, p2
|
| 49. |
Evans, S., et alia, Fever and the thermal regulation of immunity: the immune system feels the heat, Nat Rev Immunol. 2015 Jun;15(6):335-49. doi: 10.1038/nri3843. Epub 2015 May 15.
|
| 50. |
Zellner, m., et alia, Human monocyte stimulation by experimental whole body hyperthermia, Wien Klin Wochenschr. 2002 Feb 15;114(3):102-7.
|
| 51. |
Evans, S.S., et al., Fever and the thermal regulation of immunity: the immune system feels the heat, Nat. Rev. Immunol., 2015 Jun: 16(6): 335-349
|
| 52. |
Kellogg, J.H., Outlines of Practical Hydrotherapy , The Modern medicine Publishing Co., battle Creek, Mich., USA, 1922
|
| 53. |
Brooks WA, The open air treatment of influenza, Am J Public Health, 1918;8:746-750
|
| 54. |
Klein HA, The treatemnt of Spanish influenza, in Correspondence, JAMA. 1918;71(18):1510. doi:10.1001/jama.1918.02600440062019
|
| 55. |
Cherry, T.M., Influenza and maritime Quarantine in Australia, Commonwealth of Australia Quarantine Service, Service Publication 18, 1919, pages 89 to 113
|
| 56. |
Stengel, A., Influenza, in A Handbook of Practical Treatment by many Writers, W.B. Sunders Company, London, 1911
|
| 57. |
Stengel, A., Influenza, in A Handbook of Practical Treatment by many Writers, W.B. Sunders Company, London, 1911, p. 584-585
|
| 58. |
Stengel, A., Influenza, in A Handbook of Practical Treatment by many Writers, W.B. Sunders Company, London, 1911, p. 586
|
| 59. |
The Canadian formulary of unofficial preparations, The Ontario College of Pharmacy, 1921, item 76
|
Other references:
- Curson P., McCracken K., An Australian Perspective of the 1918-1919 Influenza Pandemic, CSIRO Publishing, https://www.publish.csiro.au/nb/pdf/NB06025
- Armstrong, W. G., Epidemiology and Administration, in Report on the Influenza epidemic in New South Wales in 1919, 1920 p. 154
- Porras-Gallo, M., Davis, R.A., The Spaish Influenza of 1918-1919, Perspectives from the Iberian Peninsula and the Americas, University of Rochester Press, 2014.
|
, |